What are haemorrhoids?
Haemorrhoids, also spelled as hemorrhoids or commonly referred to as ‘piles,’ are a prevalent condition characterised by the formation of lumps inside and around the anus (the back passage). They are often likened to “varicose veins” of the anus. Hemorrhoids develop when there is a weakness in the side of the anal canal, leading to thickening of the lining. As a result, veins in the area can enlarge, causing the characteristic symptoms such as bleeding, pain, and discomfort.
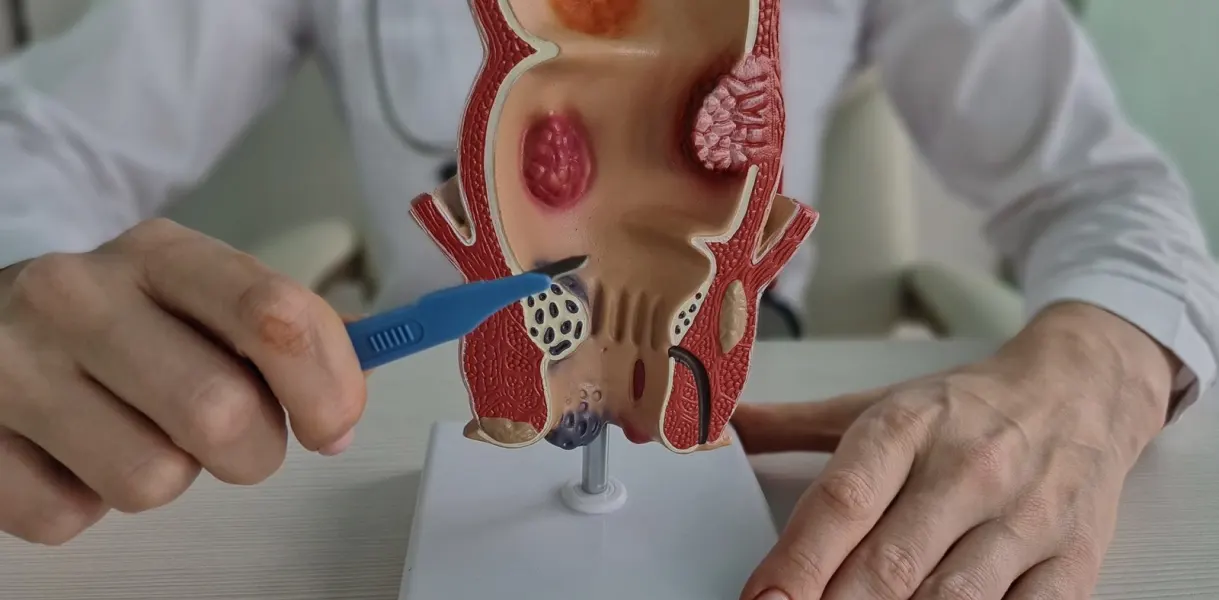
Haemorrhoids can be categorised as internal or external, depending on their location relative to the anus. Internal haemorrhoids occur inside the rectum, while external haemorrhoids develop outside the anal opening. In some cases, internal haemorrhoids may become large enough to protrude outside the anus, a condition known as prolapse. This distinction is important as it can affect the symptoms experienced and the appropriate treatment options.
While you may feel embarrassed about the thought of having haemorrhoids, it’s important to know that they’re very common, affecting as many as 75% of adults at some point during their lifetime.
What are the symptoms of haemorrhoids?
If you have haemorrhoids, you may observe bright red blood on the toilet paper or in the toilet after a bowel movement. Additionally, you might experience itchiness, discomfort, or pain around the anus. In some cases, there may be a noticeable lump that protrudes from the anus.
It’s worth noting that while many individuals with haemorrhoids may experience little to no symptoms, or only mild ones that resolve within a few days, for others, haemorrhoids can be more painful and persistent. The severity and duration of symptoms can vary greatly from person to person.


What Causes haemorrhoids?
Haemorrhoids are commonly triggered by constipation, which occurs when bowel movements are hard and difficult to pass. The act of straining during bowel movements puts pressure on the blood vessels in the anal area, leading to their swelling and inflammation.
Several factors can increase the likelihood of developing haemorrhoids, including:
- Aging: As individuals age, the tissues supporting the veins in the rectum and anus may weaken, making them more susceptible to swelling and enlargement.
- Overweight or Obesity: Excess weight can contribute to increased pressure on the pelvic area, including the veins in the anal region, leading to haemorrhoid development.
- Diarrhea: Chronic diarrhea can irritate the anal area and lead to increased frequency of bowel movements, which may contribute to the development of haemorrhoids.
- Prolonged Sitting on the Toilet: Spending long periods of time sitting on the toilet, particularly when straining to have a bowel movement, can increase pressure on the anal blood vessels and potentially lead to haemorrhoids.
- Regularly Lifting Heavy Objects: Heavy lifting can also elevate pressure in the abdominal and pelvic regions, contributing to the development of haemorrhoids.
Additionally, haemorrhoids are common during pregnancy due to several factors:
- Constipation: Constipation is a common occurrence during pregnancy, often due to hormonal changes and the pressure exerted by the growing uterus on the intestines, which can lead to the development of haemorrhoids.
- Increased Abdominal Pressure: The growing foetus places pressure on the abdomen, including the veins in the anal area, which can contribute to haemorrhoid formation.
- Increased Blood Volume: Pregnancy leads to an increase in blood volume, which can further dilate and engorge the veins in the rectal and anal regions.
- Hormonal Changes: Pregnancy hormones can relax and soften the walls of blood vessels, making them more prone to swelling and enlargement.
Moreover, there may be a genetic predisposition to developing haemorrhoids, as they tend to run in families.
Overall, while constipation is a primary trigger for haemorrhoids, several other factors, including lifestyle, pregnancy, and genetic factors, can contribute to their development. Taking steps to manage constipation and adopting healthy bowel habits can help reduce the risk of developing haemorrhoids.
What are the treatment options for haemorrhoids?
Mild symptoms of haemorrhoids may resolve on their own within a few days without the need for special treatment. However, if constipation is a contributing factor, your doctor will typically recommend measures to alleviate it.
If haemorrhoids are causing pain or discomfort, various over-the-counter medicated creams, ointments, and suppositories are available at pharmacies. These products can help relieve pain and inflammation associated with haemorrhoids. In cases of severe inflammation, your doctor may prescribe a corticosteroid cream to provide relief.
Common over-the-counter treatments for hemorrhoids include medicated creams, ointments, and suppositories designed to reduce pain and inflammation. These products are available at pharmacies without a prescription. However, for severe inflammation, a doctor may prescribe a corticosteroid cream.
In addition to topical treatments, other procedures may be recommended for internal haemorrhoids. These include:
- Injection (sclerotherapy): This involves injecting a chemical solution into the haemorrhoid, which numbs pain, stops bleeding, and causes the haemorrhoid to shrink over a period of about 4 to 6 weeks.
- Rubber band ligation: In this procedure, a tight elastic band is placed around the base of the hemorrhoid to cut off its blood supply. This causes the hemorrhoid to shrink and fall off, typically within 7 to 10 days.
In rare cases, a surgical procedure called haemorrhoidectomy may be necessary for third or fourth-degree internal haemorrhoids, large external haemorrhoids, thrombosed haemorrhoids, or combined internal and external haemorrhoids. This procedure is performed under general anesthesia and involves surgically removing the haemorrhoids.
It’s essential to consult with a healthcare professional to determine the most appropriate treatment for your specific condition and symptoms.
What is haemorrhoids banding?
Banding of haemorrhoids, also known as rubber band ligation, is a common procedure used to treat moderately sized haemorrhoids. Typically, this procedure is performed in conjunction with either a colonoscopy or a flexible sigmoidoscopy to ensure that there are no other abnormalities contributing to the bleeding further along the bowel. While banding of haemorrhoids can be done comfortably in an awake patient, it is often performed under sedation when combined with these endoscopic procedures.
During the procedure, a small elastic band is applied at the top part of the haemorrhoid above the anal canal. The band serves two main purposes: firstly, it draws the haemorrhoid internally, preventing it from prolapsing down; and secondly, it creates fixation of the haemorrhoid to the muscle underneath, thereby preventing or reducing further prolapse and bleeding. Typically, between 2 and 4 bands are required to effectively treat the haemorrhoids. It is common for patients to experience some degree of discomfort after the application of the bands.
Some patients may also experience the urge to defecate following the procedure. This sensation is related to the bands drawing up the haemorrhoids internally into the rectum, creating a feeling of rectal fullness. However, these sensations usually diminish after a couple of days.
While most banding procedures are uncomplicated, minor bleeding may occur when the haemorrhoids separate from the anal canal between days 5 and 7 after the banding. In some cases, repeat banding procedures may be necessary to achieve optimal results. Overall, banding of haemorrhoids is an effective and commonly used treatment option, but it’s essential to follow up with your healthcare provider for any post-procedural concerns or complications.
