Colonoscopies are routine procedures performed to examine the colon and rectum for any abnormalities or signs of disease, such as colorectal cancer. While the thought of a colonoscopy may be intimidating for some, it’s important to remember that the procedure itself is typically quick, and patients are usually given sedatives to help them relax and not remember much, if anything, about the procedure. So if you’ve been recommended to have a colonoscopy, there’s no need to panic. It’s a routine and important part of preventive healthcare.
At GastroMed Brisbane, the practice recommends colonoscopies to patients for various reasons, most importantly for cancer detection and prevention. This screening tool saves lives and prevents the development of colorectal cancers. If you live in Brisbane, Australia, and need a colonoscopy, it’s time to schedule an appointment with Dr. Yanez Peerbaccus.
So you’re having a Colonoscopy?
A colonoscopy is a comprehensive medical procedure performed to thoroughly examine the lower gastrointestinal tract, encompassing the rectum and colon. This diagnostic procedure is not only crucial for identifying potential issues but also serves as a means to address certain conditions, if needed.
Your gastroenterologist uses a colonoscopy to identify changes or abnormal growths in your colon (upper part of your large intestine) or your rectum (lower part of your large intestine).
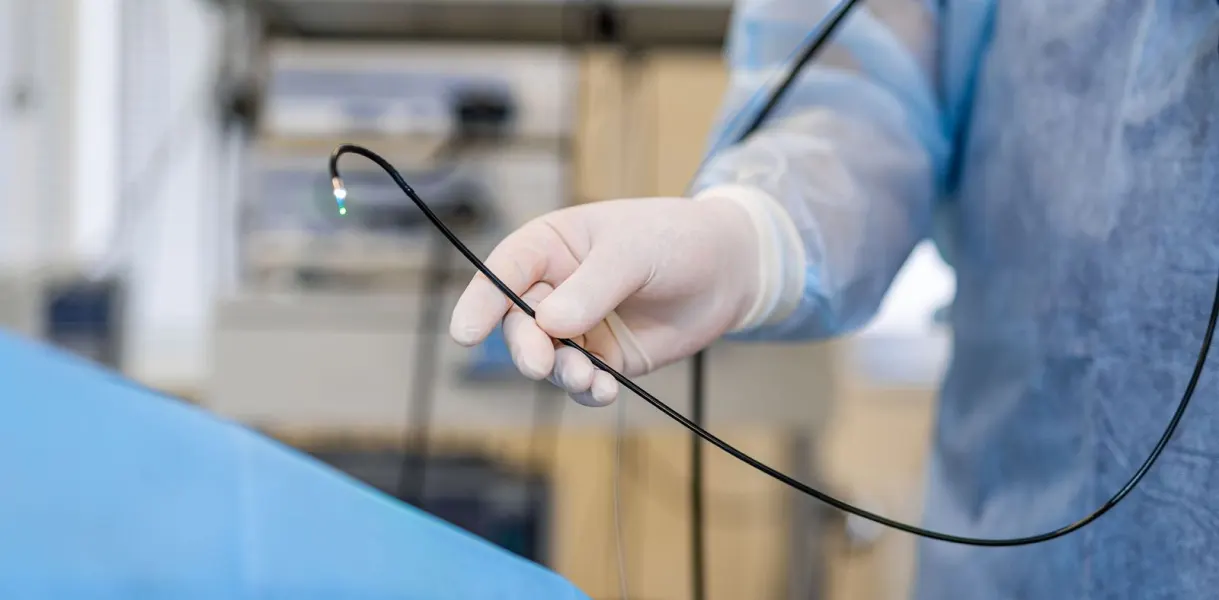
Your doctor inserts a tiny camera on the end of a long flexible tube called a colonoscope into your rectum where the image is then displayed onto a video screen. In some cases, your doctor takes a biopsy or removes polyps or abnormal tissue growths during your colonoscopy.
Who Needs a Colonoscopy
Your doctor can recommend a colonoscopy for a variety of reasons. If you have unexplained gastrointestinal symptoms like abdominal pain, rectal bleeding, chronic constipation or diarrhea, a colonoscopy allows them to investigate the source of your discomfort.
For those over 50, your doctor may recommend colonoscopy as part of your regular preventive screenings. It’s often then recommended to repeat the procedure every few years depending upon your findings.
You may also need a colonoscopy if you have a history of polyps. A follow-up scope procedure allows your doctor to look for new growths and remove any remaining polyps.
One of the primary advantages of undergoing a colonoscopy is its unparalleled efficacy in early detection of colorectal cancer, the third most common cancer worldwide. This screening procedure is widely regarded as the gold standard for assessing the presence of colon and rectal cancer due to its exceptional sensitivity and specificity. By identifying precancerous polyps during the examination, a colonoscopy offers the unique capability to remove these growths, effectively mitigating the risk of cancer development.

How Do You Prepare for a Colonoscopy?
Prior to undergoing a colonoscopy, patients are advised to disclose their complete medical history, including any pre-existing conditions and medications or supplements they are currently taking. This information enables the medical team to tailor the procedure to the patient’s specific needs and mitigate any potential risks or complications. In certain cases, certain medications or supplements may need to be temporarily discontinued prior to the procedure, as per the physician’s guidance. For instance, iron supplements are typically halted approximately one week before the colonoscopy to prevent interference with visualisation. Blood thinners such as dabigatran, rivaroxaban and Apixaban might need to be withheld from two to three days prior the procedure date. Diabetic medications such as Metformin, gliclazide, Linaglitin and Liraglutide will need to be withheld accordingly and Insulin dosage reduced.
When you have a colonoscopy, your large intestine needs to be empty. To accomplish this, your gastroenterologist gives you a special diet to follow in the days leading up to your procedure. In most cases, avoid solid food the day before the exam and consume only clear liquids. They may also request that you avoid red, blue and purple liquids. You will need to stop drinking any liquids 6 hours prior to your colonoscopy.
Your doctor may also give you a laxative. They may instruct you to take it the night before or the morning of your procedure.
What Happens During a Colonoscopy?
When you have a colonoscopy, you’re given anaesthesia to help you relax during the procedure and enter a deep sleep.
Your doctor asks you to lay on your side and draw your knees to your chest. They then insert the scope into your rectum. During a colonoscopy, the physician meticulously inspects the colon’s lining, meticulously scrutinizing for abnormalities such as inflammation, ulcers, tumors, and polyps. If any irregularities are detected, the colonoscopy provides the means to conduct various interventions on the spot. For instance, tissue samples can be collected for further analysis through biopsy, facilitating accurate diagnosis of conditions like colorectal cancer or inflammatory bowel disease. In most cases, the procedure takes 30-60 minutes. Due to the anaesthesia, you need someone to drive you home.
What happens after your procedure?
After your procedure, you will be monitored and allowed to recover from the anaesthesia. It usually takes 30 minutes to one hour. Your abdomen may be a little sore for a while, you may feel bloating or cramping right after the procedure because of air introduced into your colon during the test.
Most patients can resume a normal diet immediately afterwards.
You will go home with a copy of your procedure report, and your referring physician will receive a copy in the mail usually within one week. You will need to have someone drive you home, if you do not have a driver to take you home, your appointment will be cancelled/rescheduled. You will not be allowed to drive or operate machinery for 8 hours after the procedure and we recommend that you not attempt to go back to work that day.
What are the risk of Colonoscopy?
In Australia, serious complications from colonoscopy, including those related to polyp removal, are uncommon. Most people undergo colonoscopy without experiencing significant issues. However, the likelihood of complications can vary based on factors such as the patient’s overall health and the specific details of the procedure being performed.
One of the most serious potential complications of colonoscopy is the tearing or perforation of the bowel lining. This rare occurrence happens in approximately one out of every 1,000 cases. If a bowel perforation occurs during the procedure, it requires immediate medical attention and may necessitate surgery to repair the damaged tissue.
Occasionally, patients may experience adverse reactions to the medications used for bowel preparation or sedation. These reactions can include headaches, nausea, vomiting, or allergic responses. While uncommon, it’s important for healthcare providers to be aware of any allergies or sensitivities the patient may have to medications to minimize the risk of adverse reactions.
In some instances, a colonoscopy may not be successfully completed due to various factors, such as inadequate bowel preparation or difficulty navigating the colon. If this occurs, the procedure may need to be rescheduled for a later date to ensure a thorough examination.
While the risk of complications from colonoscopy is low, patients should be informed of the potential risks and benefits before undergoing the procedure. It’s essential for patients to communicate any concerns or questions with Dr. Yanez Peerbaccus and to carefully follow post-procedure instructions to promote optimal recovery and minimise the risk of complications.
Colonoscopies save lives, don’t put yours off. Call GastroMed Brisbane today to schedule your appointment or go online to book.
Polypectomy
Polypectomy is an endoscopic procedure to remove a growth (often benign) inside the stomach or the large bowel. This is performed whilst patients are under sedation, and involves identification of abnormal growths before removing them using endoscopic equipment (including biopsy forceps, snares or other instrument to burn off the abnormal tissue). The most important step in bowel cancer prevention is identification of polyps, and having the latest high resolution endoscopic equipment allow the Gastroenterologist to carefully look for the small, flat lesions that can be difficult to see.
Bowel polyps are quite common, with approximately half of all Australians expected to develop them at some point in their lives. However, many of these polyps go undetected, as they often do not cause noticeable symptoms. As a result, routine screening tests, such as colonoscopy, are essential for detecting and removing polyps before they have the chance to develop into cancer.
What is EMR (Endoscopic Mucosal Resection)?
Endoscopic mucosal resection, or EMR, uses a specially designed endoscope or colonoscope to remove suspect tissue or polyps from your esophagus or colon. The tissue or polyp is first injected with a solution that raises a blister, allowing your doctor to remove the tissue without damaging the rest of the esophagus or colon. The solution also helps decrease bleeding.
Suction is then used to further lift the growth up and away from surrounding tissue. A thin wire loop is slipped over the tissue, and an electric current is passed through the wire. This cuts the growth and helps to seal the wound. Once the growth is free, it’s scooped up in a small wire basket and removed from the digestive tract for analysis in the lab.
Overall, endoscopic mucosal resection represents a significant advancement in the management of large and complex polyps, offering patients a less invasive alternative to traditional surgical methods. By employing this technique, precancerous growths can effectively be eliminated, thereby reducing the risk of colorectal cancer development and enhancing patient outcomes.